Endometriosis is a poorly understood disease where the lining of the uterus (endometrium) grows in areas outside the uterus. Nobody knows why this happens although there are a number of different theories, including retrograde menstruation (bleeding back through the tubes), stromal metaplasia (abnormalities in the way tissue is placed during early foetal life) and vascular anomalies (problems with blood vessels).
It may be that all women have endometriosis at some stage during their life but most women are able to suppress its development. In most cases the areas containing endometriosis are reasonably superficial but they can at times be deeply invasive and cause significant scarring and fibrosis not unlike a malignant process.
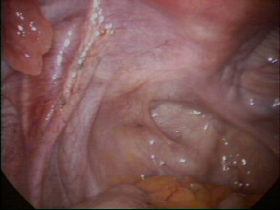
The disease can be very aggressive involving the pelvis, ovaries, bowel and bladder and even structures such as the diaphragm (breathing muscle). The symptoms can range from none to severe and include infertility, pelvic pain, irregular menstrual bleeding (particularly bleeding before the periods are due) and abdominal bloating. Pain can be very severe and be aggravated by sexual intercourse and bowel or bladder movements. Laparoscopy is the best way to diagnose the disease. Unfortunately it is not possible to diagnose with blood tests or scanning such as ultrasound or CT.
Treatment involves either drugs or surgery. Drugs serve to suppress the symptoms of the disease, but do not remove the problem and most have significant side effects. No drug has yet been shown to eradicate endometriosis or effect a long-term cure. Surgery varies depending on the extent of the disease. Traditional surgical interventions have involved either ablation or total hysterectomy and bilateral salpingoophorectomy. Ablative techniques appear to assist with mild to moderate disease but are no help in severe settings and have the potential for significant damage.
Since the depth of involvement may be particularly difficult to assess, these techniques often result in treatment to the “tip of the iceberg” with the residual disease remaining underneath the zone of treatment and ultimately “disease recurrence” (and more operations). The use of hysterectomy, which has been championed often, unfortunately has no theoretical basis and may make the situation worse by allowing invasive endometriosis to erode into both bladder and bowel. Removing the ovaries may be of value by reducing the hormonal impetus for disease progression, but does not remove the disease and substantially increases the risk of menopausal problems such as osteoporosis and ischaemic heart disease.
Excisional techniques for deeply invasive disease, whereby attempts are made to remove all the disease, have recently been demonstrated to be highly effective at relieving symptoms, with substantially less risk of recurrence than traditional therapy. If completely excised, endometriosis rarely recurs. Unfortunately the surgery is difficult and time consuming with the potential for substantial complications.
Please click on the images below for larger images and descriptions.